
The Limits of Liquid Biopsies in Ovarian Cancer Detection
In recent research presented at the European Society for Medical Oncology Gynecological Cancers Congress, a significant gap has been identified in the ability of blood-based
circulating tumor DNA (ctDNA) testing to detect KRAS mutations in patients suffering from low-grade serous ovarian cancer (LGSOC). As reported by study author Dr. Els Van Nieuwenhuysen from the University Hospitals Leuven in Belgium, this form of testing failed to identify KRAS mutations in a staggering 56% of patients who had these detectable mutations in their tumor tissues.
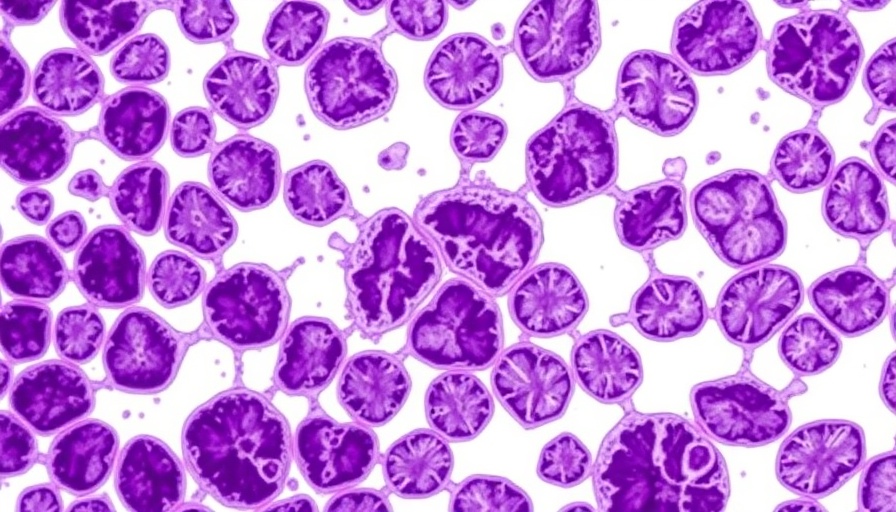
Understanding Low-Grade Serous Ovarian Cancer
LGSOC, accounting for less than 10% of all epithelial ovarian cancers, presents unique therapeutic challenges. Unlike more aggressive high-grade ovarian cancers, LGSOC tumors are primarily driven by mutations in the RAS/MAPK signaling pathway, with KRAS mutations present in approximately 30% of the patient population. Conventional chemotherapy treatments show minimal effectiveness in these cases, producing response rates between 0% and 13%.
Comparative Safety: Traditional Methods vs. Liquid Biopsies
The RAMP-201 trial analyzed blood samples from 65 patients with confirmed LGSOC, revealing that only 32% had detectable ctDNA levels using the Tempus xF panel, which evaluates over 100 cancer-related genes inclusive of KRAS. This contrasted sharply with the traditional tumor tissue analysis, which reliably detected the same mutations. Van Nieuwenhuysen emphasized that the low detection rate of KRAS from blood samples raises significant concerns regarding treatment decisions being based on potentially faulty data, jeopardizing patient care and therapy selection.
Current Approvals and Implications for Treatment
Despite the shortcomings of blood-based testing, there are advancements in treatment for LGSOC. The FDA's accelerated approval of a combination therapy—avutometinib (a RAF/MEK inhibitor) and defactinib (a FAK inhibitor)—for patients with KRAS-mutated recurrent LGSOC highlights the urgency of accurate mutation detection for effective treatment outcomes. For patients with KRAS mutations, the combination therapy has exhibited a response rate of 44%, significantly better than the 17% rate in those who are KRAS wild-type.
What This Means for Patients and Future Research
The findings from this study underline the necessity for continued reliance on traditional tumor tissue analysis when it comes to making treatment decisions for LGSOC. While the potential of liquid biopsies is recognized and ongoing research aims to enhance their reliability, it is clear that current methods fall short for this specific cancer type. Future studies may focus on improving ctDNA methodologies to ensure that they can accurately reflect the mutation profiles essential for patient care.
Conclusion: The Evolving Landscape of Cancer Detection
This study's implications extend beyond just ovarian cancer treatment; they challenge broader trends in liquid biopsy adoption for cancer detection. Patients, clinicians, and researchers alike must navigate these complexities carefully, ensuring that advancements do not inadvertently overshadow the proven methodologies that still play a crucial role in diagnosis and treatment planning. As research continues, the hope is to bridge these gaps, enhancing patient outcomes while fully optimizing the potential of emerging technologies.
 Add Row
Add Row  Add
Add 



 Add Row
Add Row  Add
Add 

Write A Comment